The most contentious aspect of the medical marijuana debate is not whether marijuana
can alleviate particular symptoms, but rather the degree of harm associated with its use.
This chapter thus explores the negative health consequences of marijuana use, first with
respect to drug abuse, then from psychological perspective, and finally from a
physiological perspective.
- The most commonly reported effects of smoked marijuana are a sense of well-being or
euphoria and increased talkativeness and laughter alternating with periods of
introspective dreaminess followed by lethargy and sleepiness (see reviews by Adams and
Martin I 996, and Hall 1994 and 1998 1, 58, 59). A characteristic feature of a
marijuana "high" is a distortion in the sense of time associated with deficits
in short-term memory and learning. A marijuana smoker typically has a sense of enhanced
physical and emotional sensitivity' including a feeling of greater interpersonal
closeness. The most obvious behavioral abnormality displayed by someone under the
influence of marijuana is difficulty in carrying on an intelligible conversation, perhaps
because of an inability to remember what was just said even a few words earlier.
- The high associated with marijuana is not generally claimed to be integral to its
therapeutic value. But mood enhancement, anxiety reduction, and mild sedation can be
desirable qualities in medications particularly for patients suffering pain and anxiety.
Thus, although the psychological effects of marijuana are merely side effects in the
treatment of some symptoms, they might contribute directly to relief of other symptoms.
They also must be monitored in controlled clinical trials to discern which effect of
cannabinoids is beneficial. These possibilities are discussed later under the discussions
of specific symptoms in chapter 4.
- The effects of various doses and routes of delivery of THC are shown in table 3.1.
3.2
Table 3.1 Psychoactive Doses of THC in Humans
| THC Delivery System |
THC Dose Administered |
Resulting Level of THC in Plasma |
Subjects' Reactions |
Reference |
| One 2.75% THC cigarette smoked |
0.32 mg/kg* |
50-100 ng/ml |
At higher level subjects felt 100% "high" and psychomotor performance
is decreased. At 50 ng/ml subjects felt about 50% "high" |
Heishman and coworkers 1990 |
| 1 gm marijuana cigarette smoked (2% or 3.5% THC) |
0.25-0.50 mg/kg* |
Not measured |
Enough to feel psychological effects of THC |
Kelly and coworkers 1993 |
| 19 mg THC cigarette smoked (approx 1.9% THC) |
Approx. 0.22 mg/kg** |
100 ng/ml |
Subjects felt "high" |
Ohlsson and coworkers 1980 |
| 5 mg THC injected i.v. |
Approx. 0.06 mg/kg** |
100 ng/ml |
Subjects felt "high" |
| Chocolate chip cookie containing 20 mg THC |
Approx. 0.24 mg/kg |
8 ng/ml |
Subjects rated "high" as only about 40% |
| 19 mg THC cigarette smoked to "desired high" |
12 mg was smoked (7 mg remained in cigarette butt) |
85 ng/ml (after 3 min.) 35 ng/ml (after 15 min.) |
Subjects felt "high" after 3 minutes, and maximally high after 10-20 minutes
(average self ratings of 5.5 on a 10-point scale) |
Lindgren and coworkers 1981 |
| 5 mg THC injected i.v. |
0.06 mg/kg*** |
300 ng/ml (after 3 min.) 65 ng/ml (after 15 min.) |
Subjects felt maximally "high" after 10 minutes (average self ratings of 7.5
on a 10-point scale) |
* Subjects' weights and cigarette weights were not given. Calculation based on 85 kg
body weight, and 1g cigarette weight. Note that some THC would have remained in the
cigarette butt and some would have been lost in side-stream smoke, so these represent
maximal possible doses administered. Actual doses would have been slightly less.
** Based on estimated average weight of 85 kg for 11 men aged 18-35 years.
*** Based on approximately weight of 80 kg (subjects included men and women).
3.3
Adverse mood reactions
- Although euphoria is the more common reaction to smoking marijuana, adverse mood
reactions can occur. Such reactions occur most frequently in inexperienced users after
large doses of smoked or oral marijuana. They usually disappear within hours and respond
well to reassurance and a supportive environment. Anxiety and paranoia are the most common
acute adverse reactions, 58 others include panic, depression, dysphoria,
depersonalization, delusions, illusions, and hallucinations.) 1, 40, 65, 68 Of
regular marijuana smokers, 17% report that they have experienced least one of the
symptoms, usually early in their use of marijuana. 144 Those observations are
particularly relevant for the use of medical marijuana in people who have not previously
used marijuana.
Drug dynamics
- There are many misunderstandings about drug abuse and dependence (see reviews by O'Brien
113 and Goldstein 54). The terms and concepts used in this report
are as defined in the most recent Diagnostic and Statistical Manual of Mental Disorders
(DSM-IV3 ), the most influential system in the United States for diagnoses of
mental disorders, including substance abuse (see box on definitions). Tolerance,
dependence, and withdrawal are often presumed to imply abuse or addiction, but this is not
the case. Tolerance and dependence are normal physiological adaptations to repeated use of
any drug. The correct use of prescribed medications for pain, anxiety, and even
hypertension commonly produces tolerance and some measure of physical dependence.
- Even a patient who takes a medicine for appropriate medical indications and at the
correct dosage can develop tolerance, physical dependence, and withdrawal symptoms if the
drug is stopped abruptly rather than gradually. For example, a hypertensive patient
receiving a beta-adrenergic receptor blocker, such as propranolol, might have a good
therapeutic response; but if the drug is stopped abruptly, there can be a withdrawal
syndrome that consists of tachycardia and a rebound increase in blood pressure to a point,
temporarily higher than before administration of the medication began.
- Because it is an illegal substance, some people consider any use of marijuana as
substance abuse. However, this report uses the medical definition; that is, substance
abuse is a maladaptive pattern of repeated substance use manifested by recurrent and
significant adverse consequences.3 Substance abuse and dependence are both
diagnoses of pathological substance use. Dependence is the more serious diagnosis and
implies compulsive drug use that is difficult to stop despite significant
substance-related problems (see box on criteria for substance dependence).
3.4
DEFINITIONS
Addiction. Substance dependence.
Craving refers to the intense desire for a drug and is the most difficult aspect
of addiction to overcome.
Physiological dependence is diagnosed when there is evidence of either tolerance
or withdrawal; it is sometimes, but not always, manifested in substance dependence
Reinforcement. A drug - or any other stimulus -- is referred to as a reinforcer
if exposure to it is followed by an increase in frequency of drug-seeking behavior. The
taste of chocolate is a reinforcer for biting into a chocolate bar. Likewise, for many
people, the sensation experienced after drinking alcohol or smoking marijuana is a
reinforcer.
Substance dependence is a cluster of cognitive, behavioral, and physiological
symptoms indicating that a person continues use of the substance despite significant
substance-related problems.
Tolerance is the most common response to repetitive use of a drug and can be
defined as the reduction in responses to the drug after repeated administrations.
Withdrawal. The collective symptoms that occur when the drug is abruptly
withdrawn are known as withdrawal syndrome and are often the only evidence of physical
dependence.
3.5
DSM-IV Criteria for Substance Dependence
- A maladaptive pattern of substance use. leading to clinically significant impairment or
distress as manifested by three (or more) of the following, occurring at any time in the
same l2-month period:
(1) Tolerance, as defined by either of the following:
(a) A need for markedly increased amount of the substance to achieve
intoxication or desired effect.
(b) Markedly diminished effect with continued use of the same amount of the
substance.
(2) Withdrawal, as defined by either of the following:
(a) The characteristic withdrawal syndrome for the substance to achieve
intoxication or desired effect.
(b) The same (or closely related) substance is taken to relieve or avoid
withdrawal symptoms.
(3) The substance is often taken in larger amounts or over a longer period than
was intended.
(4) There is a persistent desire or unsuccessful efforts to cut down or control
substance use.
(5) A great deal of time is spent in activities necessary to obtain the
substance
(e.g. visiting multiple doctors driving long distances), use the substance
(e.g., chain-smoking), or recover from its effects.
(6) Important social occupational, or recreational activities are given up or
reduced because of substance use
(7) The substance use is continued despite knowledge of having a persistent or
recurrent physical or psychological problem or exacerbated by the substance
(e.g., current cocaine use despite recognition of cocaine-induced depression or continued
drinking despite recognition that an ulcer was made worse by alcohol consumption).
Substance abuse with physiological dependence is diagnosed if there is
evidence of tolerance or withdrawal.
Substance abuse without physiological dependence is diagnosed if there is
no evidence of tolerance or withdrawal.
3.6
Reinforcement
- Drugs vary in their ability to produce good feelings in the and the more strongly
reinforcing a drug is, the more likely it will be abused (G. Koob, IOM workshop).
Marijuana is indisputably reinforcing for many people. The reinforcing properties of even
so mild a stimulant as caffeine are typical of reinforcement by addicting drugs (reviewed
by Goldstein 54 in 1994). Caffeine is reinforcing for many people at low doses
(100-200 ma' the average amount of caffeine in one to two cups of coffee), and aversive at
high doses (600 mg the average amount of caffeine in six cups of coffee). The reinforcing
effects of many drugs are different for different people. For example, caffeine was most
reinforcing for test subjects who scored lowest on tests of anxiety but tended not to be
reinforcing for the most anxious subjects.
- As an argument to dispute the abuse potential of marijuana, some have cited the
observation that animals do not willingly self-administer THC, as they will cocaine. Even
if that were true, it would not be relevant to human use of marijuana. The value in animal
models of drug self-administration is not that they are necessary to show that a drug is
reinforcing, but rather that they provide a model in which the effects of a drug can be
studied. Furthermore, THC is indeed rewarding to animals at some doses but, like many
reinforcing drugs, is aversive at high doses (4.0 mg/kg). 92 Similar effects
have been found in experiments conducted in animals outfitted with intravenous catheters
that allow them to self-administer WIN 55,212, a drug that mimics the effects of THC. 99
- A specific set of neural pathways has been proposed to be a "reward system"
that underlies the reinforcement of drugs of abuse 51 and other pleasurable
stimuli. 51 Reinforcing properties of drugs are associated with their ability
to increase concentrations of particular neurotransmitters in areas that are part of the
proposed brain reward system. The median forebrain bundle and the nucleus accumbens are
associated with brain reward pathways. 87 Cocaine, amphetamine, alcohol,
opioids, nicotine, and THC 143 all increase extracellular fluid dopamine in the
nucleus accumbens region (reviewed by Koob 87 and Nestler 109 in
1997). However, it is important to note that brain reward systems are not strictly
"drug reinforcement centers". Rather, their biological role is to respond to a
range of positive stimuli, including sweet foods and sexual attraction.
Tolerance
- The rate at which tolerance to the various effects of any drug develops is an important
consideration for its safety and efficacy.. For medical use, tolerance to some effects of
cannabinoids might be desirable. Differences in the rates at which tolerance to the
multiple effects of a drug develops can be dangerous. For example, tolerance to the
euphoric effects of heroin develops faster than tolerance to its
3.7
respiratory depressant effects, so heroin users tend to increase their daily doses to
reach their desired level of euphoria, thereby putting them at risk for respiratory
arrest. Because tolerance to the various effects of cannabinoids might develop at
different rates, it is important to evaluate independently their effects on mood, motor
performance, memory, and attention, as well as any therapeutic use under investigation.
- Tolerance to most of the effects of marijuana can develop rapidly after only a few
doses, and it also disappears rapidly. Tolerance to large doses has been found to persist
in experimental animals for long periods after cessation of drug use. Performance
impairment is less among people who use marijuana heavily than it is among those who use
marijuana only occasionally, 29, 103, 123 possibly because of tolerance. Heavy
users tend to reach higher plasma concentrations of THC than light users after similar
doses of THC, arguing against the possibility that heavy users show less performance
impairment because they somehow absorb less THC (perhaps due to differences in smoking
behavior). 94
- There appear to be variations in the development of tolerance to the different effects
of marijuana and oral THC. For example, a group of daily marijuana smokers participated in
a residential laboratory study to compare the development of tolerance to THC pills and to
smoked marijuana. 60, 61 One group was given marijuana cigarettes to smoke four
times per day for four consecutive days. Another group was given THC pills on the same
schedule. During the 4-day period, both groups became tolerant to feeling "high"
and what they reported as a "good drug effect." In contrast, neither group
became tolerant to the stimulatory effects of marijuana or THC on appetite. Note that
tolerance does not mean the drug no longer produced those effects, simply that the effects
were less at the end than they were at the beginning of the 4-day period. The marijuana
smoking group reported feeling "mellow" after smoking, and did not show
tolerance to this effect. Interestingly, the group who took THC pills did not report
feeling "mellow," a difference that was also reported by many people who
described their experiences to the IOM study team.
- The oral and smoked doses were designed to deliver roughly equivalent amounts to THC to
the subject. Each smoked marijuana dose consisted of five 10 second puffs of a 3.1%
marijuana cigarette; the pills contained 30 mg of THC. Both groups also received placebo
drugs during other four-day periods. While the dosing of the two groups was comparable,
different routes of administration result in different patterns of drug effect. The peak
effect of smoked marijuana is felt within minutes, and declines sharply after 30 minutes, 67,
94; the peak effect of oral THC is usually not felt until about an hour and lasts
for several hours. 117
Withdrawal
A distinctive marijuana and THC withdrawal syndrome has been identified, but it is mild
and subtle compared to the profound physical syndrome of alcohol or heroin withdrawal 31
73 The marijuana withdrawal syndrome includes restlessness, irritability, mild
agitation, insomnia, sleep EEG disturbance, nausea, and cramping
3.8
(table 3.2). This syndrome, however, has only been reported in a group of adolescents
in treatment for substance abuse problems or in a research setting where subjects were
given marijuana or THC on a daily basis 73
3.9
Table 3.2 Drug Withdrawal Symptoms
| Nicotine |
Alcohol |
Marijuana |
Cocaine |
Opioids
(e.g. heroin) |
| |
| Restlessness Irritability
Dysphoria
Impatience, hostility
Depression
Difficulty concentrating
Anxiety
Decreased heart rate
Increased appetite or weight gain |
Tremor Irritability
Nausea
Sleep disturbance
Tachycardia
Perceptual distortion
Hypertension
Sweating
Seizures
Alcohol craving
Delirium tremens (severe agitation, confusion, visual hallucinations, fever, profuse
sweating, nausea, diarrhea, dilated pupils) |
Restlessness Irritability
Mild agitation
Sleep EEG disturbance
Insomnia
Nausea, Cramping |
Dysphoria Depression
Bradycardia
Sleepiness, fatigue
Cocaine craving |
Restlessness Irritability
Increased sensitivity to pain
Dysphoria
Insomnia, anxiety
Muscle aches
Nausea, cramps
Opioid craving |
Table legend. This summary of withdrawal symptoms is from O'Brien's 1996 review. 112
In addition to the established symptoms listed above, two recent studies have reported
several more. A group of adolescents under treatment for conduct disorders also reported
fatigue and illusions or hallucinations after marijuana abstinence (this study is
discussed further under the section on "Prevalence and Predictors of
Dependence"). 31 In a residential study of daily marijuana users,
withdrawal symptoms included sweating and rhinorrhea (runny nose), in addition to those
listed above (this study is discussed further under the section on "Tolerance").
31
3.10
- Withdrawal symptoms have been observed in carefully controlled laboratory studies of
people following use of both oral THC and smoked marijuana (Haney and coworkers in press).
In one study, subjects were given very high doses of oral THC: 180-210 mg per day for 10
to 20 days, roughly equivalent to smoking 9-10 two percent THC cigarettes per day. 73
During the abstinence period at the end of the study, the study subjects were irritable
and showed insomnia, rhinorrhea (runny nose), sweating, and decreased appetite. The
withdrawal symptoms, however, were short-lived. After four days they had abated. This time
course contrasts with another study in which lower doses of oral THC were used (80-120
mg/day for four days), and withdrawal symptoms were still near maximal after four days
(Haney and coworkers, in press).
- In animals, simply discontinuing chronic heavy dosing of THC does not reveal withdrawal
symptoms However, in animal studies, the removal of THC from the brain can be made abrupt
by another drug that blocks THC at its receptor when administered at the same time the
chronic THC is withdrawn. In this case, the withdrawal syndrome is quite pronounced, and
the behavior of the animals becomes hyperactive and disorganized. 152 The
half-life of THC in brain is approximately one hour. 16, 24 Although traces of
THC can remain in the brain for much longer periods, the amounts are not physiologically
significant. Thus, the lack of a withdrawal syndrome seen if THC is abruptly withdrawn
without the addition of a receptor blocking drug is not likely due to a prolonged decline
in brain levels.
Craving
- Craving, the intense desire for a drug, is the most difficult aspect of addiction to
overcome. Research on craving has focused on nicotine, alcohol, cocaine, and opiates, but
has not specifically addressed marijuana. 114 Thus, while this section briefly
reviews what is known about drug craving, its relevance to marijuana use has not been
established.
- Most individuals who suffer from addiction relapse within a year of abstinence, and they
often attribute their relapse to craving. 57 As addiction develops, craving
increases even as maladaptive consequences accumulate. Animal studies indicate that the
tendency to relapse is based on changes in brain function that continue for months or
years after the last use of the drug" 114 Whether the neurobiology changes
during the manifestation of an abstinence syndrome remains an unanswered question in drug
abuse research. 87 The liking of sweet foods, for example, is mediated by
certain opioid forebrain systems and by brain-stem systems, whereas wanting seems to be
mediated by ascending dopamine neurons that project to the nucleus accumbens. 108
- Anti-craving medications have been developed for nicotine and alcohol. The
antidepressant, bupropion, blocks nicotine craving, while naltrexone blocks alcohol
craving. 114 Another category of addiction medication includes drugs that block
3.11
another drug's effects. Some of these addiction medication drugs also block craving.
For example, methadone blocks the euphoria effects of heroin and also reduces craving.
Marijuana Use and Dependence
Prevalence of Use
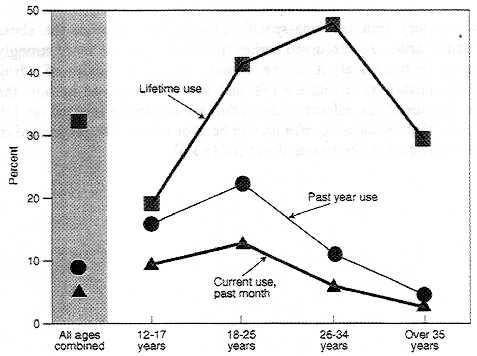
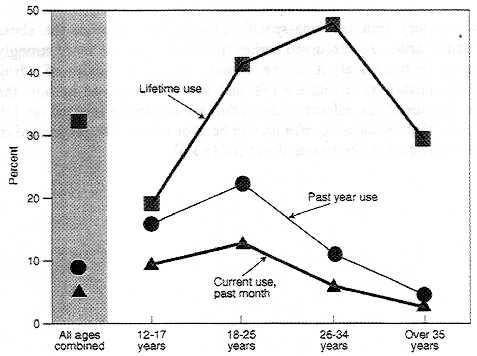
- Millions of Americans have tried marijuana, but most are not regular users. In 1996,
68.6 million people or 32 % of the U.S. population over 12 years old had tried marijuana
or hashish at least once in their lifetime, but only 5 % were current users. 131 Marijuana
use is most prevalent among 18-25 year olds and declines sharply after age 34 (figure
3.1). 76, 131 Among adolescents, whites are more likely than blacks to use
marijuana' although this difference decreases by adulthood. 131
- Most people who have used marijuana did so first during adolescence. Social influences,
such as peer pressure and Prevalence of use by peers, are highly predictive of initiation
into marijuana use. 9 Initiation is not, of course, synonymous with continued
or even regular use. A cohort of 456 students who experimented with marijuana during their
high school years were surveyed about their reasons for initiating, continuing, and
stopping drug use. 9 Students who began as heavy users were excluded from the
analysis, Those who did not become regular marijuana users cited two types of reasons for
discontinuing. The first was related to their health and well-being, that is, they felt
marijuana was bad for their health or their family and work relationships. The second type
was based on age-related changes in circumstances, including increased responsibility and
less regular contact with other marijuana users. Interestingly, among high school students
who quit, parental disapproval was a stronger influence than peer disapproval in
discontinuing marijuana use. In the initiation of marijuana use, the reverse was true. The
reasons cited by those who continued to use marijuana were to "get in a better mood
or feel better.'' Social factors were not a significant predictor of continued use after
initiation. Data on young adults show similar trends. Those who use drugs in response to
social influences are more likely to stop using them than those who also use drugs for
psychological reasons. 79
- The age distribution of marijuana users among the general population contrasts with that
of medical marijuana users. Marijuana use generally declines sharply after age 34, whereas
medical marijuana users tend to be over 35 (figure 3.1). This raises the question as to
what, if any, relationship exists between abuse and medical use of marijuana, however,
there are no studies reported in the scientific literature that address this question.
3.12
Figure 3.1 Age distribution of marijuana users among the general population
3.13
Prevalence and Predictors of Drug Dependence
- Many factors influence the likelihood that a particular person will become a drug abuser
or an addict: the user, the environment, and the drug are all important factors (table
3.3). 113 The first two categories apply to potential abuse of any substance;
that is, someone who is vulnerable to drug abuse for individual reasons, and who finds
themselves in an environment that encourages drug abuse, is initially likely to abuse the
most readily available drug - regardless of its unique set of effects on the brain.
- The third category includes drug-specific effects that influence the abuse liability of
a particular drug. As discussed earlier in this chapter, the more strongly reinforcing a
drug is, the more likely it will be abused. The abuse liability of a drug is enhanced by
how quickly its effects are felt, and this is determined by how the drug is delivered. In
general, the effects of drugs that are inhaled or injected are felt within minutes, those
that are ingested take half an hour or more. The proportion of people who become addicted
varies among drugs (table 3.4).
3.14
Table 3.3 Factors that are correlated with drug dependence
- Individual Factors
- Pharmacological effects of the drug
- Gender
- Age
- Genetic factors
- Individual risk-taking propensities
- History of prior drug use
- Environmental Factors
- Availability of the drug
- Acceptance of the use of that drug within society
- Balance of social reinforcements and punishments for use
- Balance of social reinforcements and punishments for abstinence
Source: Crowley and Rhine (1985)32
Table legend. Factors that can influence the likelihood that an individual will become
dependent on a drug.
3.15
Table 3.4 Prevalence of Drug Use and Dependence Among the General Population
| Drug Category |
Proportion Who have Ever Used Different Types of Drugs |
Proportion Of Users That Ever Became Dependent |
| Tobacco |
76 % |
32 % |
| Alcohol |
92 % |
15 % |
Marijuana
(including hashish) |
46 % |
9 % |
Anxiolytics
(including sedatives
and hypnotic drugs) |
13 % |
9 % |
| Cocaine |
16 % |
17 % |
| Heroin |
2 % |
23 % |
Table legend. The table shows estimates for the proportion of people among the
general population who used or became dependent on different types of drugs. The proportion
of users that ever became dependent includes anyone who was ever dependent -
whether it was for a period of weeks or years - and thus includes more than those who are
currently dependent. The diagnosis of drug dependence used in this study was based on
DSM-III-R criteria. 2 Adapted from table 2 in Anthony and coworkers (1994). 8
- Compared to most other drugs listed in this table, dependence among marijuana users is
relatively rare. This might be due to differences in the specific drug effects; in the
availability of, or penalties associated with the use of, the different drugs -- or, some
combination of these possible reasons.
- Note that the percent listed are from the Epidemiological Catchment Area study, and (of
people who ever used marijuana) (46 %), are higher than that reported by the National
Household Survey on Drug abuse (32%). The differences are likely due to different survey
methods (for discussion see Kandel 199275).
3.16
- Daily use of most illicit drugs is extremely rare in the general population. In 1989
daily use of marijuana among high school seniors was less than that of alcohol (2.9% and
4.2 %, respectively) 75
- Drug dependence is more prevalent in certain sectors of the population than others. Age,
gender, and race or ethnic group are all significant factors.8 Excluding tobacco and
alcohol, the following trends of drug dependence are statistically sigruficant:8 Men are
1.6 times more likely than women to become drug dependent. Non-Hispanic whites are about
twice as likely as African-Americans to become drug dependent. (The difference between
non-Hispanic and Hispanic whites was not significant.) Lastly, people aged 25-44 years are
more than three times as likely as those over 45 years to become drug dependent.
- More often than not, drug dependence co-occurs with one or more other psychiatric
disorders. The majority of individuals diagnosed with a drug dependence disorder are also
diagnosed with another psychiatric disorder (76 % of men, 65 % of women). 75
The most frequent co-occurring disorder is alcohol abuse; 60 % of men and 30 % for women
diagnosed as drug dependent also abuse alcohol. For women who are drug dependent, phobic
disorders and major depression are almost equally common (29 % and 28 %, respectively).
Note that this study distinguished only between alcohol, nicotine and "other
drugs," the category that included marijuana. The frequency with which drug
dependence and other psychiatric disorders co-occur might not be the same for marijuana
and other drugs that were included in that category of "other drugs."
- A strong association between drug dependence and antisocial personality or its
precursor, conduct disorder, is also widely reported in children and adults (reviewed by
Robins 125 in 1998). Although the causes of this association are still
uncertain, Robins recently concluded that it is more likely that conduct disorders
generally lead to substance abuse than the reverse. 125 Such a trend might,
however, depend on the age at which the conduct disorder is manifested.
- A longitudinal study by Brooks and coworkers indicated that while childhood conduct
disorder may lead to later drug use for older adolescents there is no evidence that
depression, anxiety, or conduct disorders precede heavy drug use. 18 Rather,
the drug use preceded the psychiatric disorders. In contrast to tobacco and other illicit
drugs, moderate (less than once a week, more than once a month) to heavy marijuana use did
not predict anxiety or depressive disorders, but was consistent with those other drugs in
predicting antisocial personality disorder. The rates of disruptive disorders increased
with increased levels of drug use. Thus, heavy drug use among adolescents can be a warning
sign for later psychiatric disorders, whether it is an early manifestation of symptoms for
those disorders or a causal factor remains to be determined.
3.17
- Psychiatric disorders are more prevalent among adolescents who use drugs including
alcohol and nicotine. 78 Table 3.5 indicates that daily cigarette smoking among
adolescent boys is associated with an approximately tenfold increase in the likelihood of
being diagnosed with a psychiatric disorder compared to those who do not smoke. Note,
however, that the table does not compare equivalent intensity of use among the different
drug classes. Thus, although daily cigarette smoking among adolescents is more strongly
associated with psychiatric disorders than is any use of illicit substances, it does not
follow that this comparison is true for every amount of cigarette smoking. 78
3.18
Table 3.5 Psychiatric disorders associated with drug use among children
| Relative prevalence of diagnoses for psychiatric disorders associated
with drug use among children |
| . |
Relative Prevalence Estimates |
| Drug Use |
Boys |
Girls |
| Weekly alcohol use |
6.1 |
1.6 (n.s.) |
| Daily cigarette smoking |
9.8 |
2.1 (n.s.) |
| Any illicit substance use |
3.2 |
5.3 |
Table legend. The subjects ranged in age from 9-18 years, with an average age of
13 years.
A ratio of one means that the relative prevalence of the disorder is equal among those
who do and those who do not use the particular type of drug, that is, there is no
measurable association. A ratio greater than one indicates that the factor is associated.
Thus boys who smoke daily are as almost ten times more often diagnosed as having a
psychiatric disorder (not including substance abuse) as those who smoke less. Substance
abuse was excluded from this analysis since the subjects being analyzed were already
grouped by their high drug use. Except where noted (n.s.) all values are statistically
significant..
Data are from table 4 in Kandel and coworkers 1997 78
3.19
Marijuana Dependence
- Few marijuana users become dependent (table 3.4), but those who do encounter problems
similar to those associated with dependence on other drugs.19 142 The severity
of dependence appears to be less among people who use only marijuana than among those who
abuse cocaine or abuse marijuana with other drugs (including alcohol). 19, 142
- Data gathered in 1990-1992 from the National Comorbidity Study of over 8,000 persons
aged 15-54 years indicate that 4.2 % of the general population were dependent on marijuana
at one time in their life. 8 Similar results for the frequency of substance
abuse among the general population were obtained from the Epidemiological Catchment Area
Program, a survey of over 19,000 people. Based on data collected in the early 1980s for
that study, 4.4% of adults have, at one time, met the criteria for marijuana dependence.
For comparison, 13.8% of adults met the criteria for alcohol-dependence and 36.0% met them
for tobacco. After alcohol and nicotine, marijuana was the substance most frequently
associated with a diagnosis of substance dependence.
- In a fifteen-year study begun in 1979 of 1,201 adolescents and young adults in suburban
New Jersey, 7.3% of those subjects, at one time, met the criteria for marijuana
dependence, indicating that the rate of marijuana dependence might be even higher in some
groups of adolescents and young adults than for the general population. 70
Adolescents meet the criteria of drug dependence at lower rates of marijuana use than do
adults, suggesting that they are more vulnerable to dependence than adults 25
(see box on Criteria for Substance Abuse).
- Youths who are already dependent on other substances are particularly vulnerable to
marijuana dependence. For example, Crowley and coworkers 31 interviewed a group
of 229 adolescent patients in a residential treatment program for delinquent,
substance-involved youth, and found that those patients were dependent on an average of
3.2 different substances. The adolescents in this study had previously been diagnosed as
dependent on at least one substance (including nicotine and alcohol) and had three or more
conduct disorder symptoms during their life. Among those troubled adolescents, about 83%
of those who had previously used marijuana at least six times went on to develop marijuana
dependence. Approximately equal numbers of youths in this study were diagnosed as
marijuana dependent as were diagnosed as alcohol-dependent, fewer were diagnosed as
nicotine-dependent. However, comparisons between the dependence potential of different
drugs should be made cautiously. The probability that a particular drug will be abused is
influenced by many factors, including the specific drug effects and availability of the
drug.
3.20
- Although parents often state that marijuana caused their children to be rebellious, the
troubled adolescents in the study by Crowley and coworkers developed conduct disorders
before marijuana abuse. This is consistent with reports showing that the more symptoms of
conduct disorders children have, the younger they begin drug abuse, 126 and
that the younger they begin drug use, the more likely it is to be followed by abuse or
dependence. 124
- Genetic factors are known to play a role in the likelihood of substance abuse for drugs
other than marijuana, 7 128 and it is not unexpected that genetic factors might
play a role in the marijuana experience, including the likelihood of abuse. A study of
over 8,000 male twins listed in the Vietnam Era Twin Registry indicated that genes have a
significant influence on whether an individual finds the effects of marijuana pleasant. 96
Not surprisingly, individuals who found marijuana to be pleasurable used it more often
than those who found it unpleasant. The study suggested that, although social influences
play an important role in the initiation of use, individual differences - perhaps
associated with the brain's reward system - influence whether an individual will continue
using marijuana. Similar results were found in a study of female twins. 85
Family and social environment strongly influenced the likelihood of ever using marijuana,
but had little impact on the likelihood of heavy use or abuse. The latter were more
influenced by genetic factors. These results are consistent with the finding that the
degree to which rats find THC rewarding is genetically based. 91
- In sum, although few marijuana users develop dependence, some do. But, they appear to be
less likely to do so than users of other drugs (including alcohol and nicotine), and
marijuana dependence appears to be less severe than it is for other drugs. Drug dependence
is more prevalent in certain sectors of the population, but no group has been identified
as being particularly vulnerable to the drug-specific effects of marijuana. Adolescents,
especially troubled adolescents, and people with psychiatric disorders (including
substance abuse) appear to more likely than the general population to become dependent on
marijuana.
- If marijuana or cannabinoid drugs were approved for therapeutic uses, it would be
important to consider the possibility of dependence, particularly for patients in high
risk groups for substance dependence. Certain controlled substances that are approved
medications produce dependence after long term use. This is, however, a normal part of
patient management and does not generally present undue risk to the patient.
3.21
- The fear that marijuana use might cause, as opposed to merely precede, the use of drugs
that are more harmful of great concern. Judging from comments submitted to the IOM study
team, this appears to be an even greater concern than the harms directly related to
marijuana itself. The discussion that marijuana is a gateway drug implicitly recognizes
that other illicit drugs might inflict greater damage to health or social relations than
marijuana. Although the scientific literature generally discusses drug use progression
between a variety of drug classes, including alcohol and tobacco, the public discussion
has focused on marijuana as a gateway drug that leads to abuse of more harmful illicit
drugs such as cocaine and heroin.
- There are strikingly regular patterns in the progression of drug use from adolescence to
adulthood. Because it is the most widely used illicit drug, marijuana is predictably the
first illicit drug most people encounter. Not surprisingly, most users of other illicit
drugs have used marijuana first. 80, 81 In fact, most drug users do not begin
their drug use with marijuana; they begin with alcohol and nicotine and usually when they
are too young to do so legally. 81, 89
- The gateway analogy evokes two ideas that are often confused. The first, more often
referred to as the stepping stone hypothesis, is the idea that progression from marijuana
to other drugs arises from pharmacological properties of marijuana itself. 81
The second interpretation is that marijuana serves as a gateway to the world of illegal
drugs in which youths have greater opportunity and are under greater social pressure to
try other illegal drugs. This is the interpretation most often used in the scientific
literature, and is supported by -- although not proven by the available data.
- The stepping stone hypothesis applies to marijuana only in the broadest sense. People
who enjoy the effects of marijuana are, logically, more likely to be willing to try other
mood-altering drugs than are people who are not willing to try marijuana or who dislike
its effects. In other words, many of the factors associated with a willingness to use
marijuana are, presumably, the same as those associated with a willingness to use other
illicit drugs. Those factors include physiological reactions to the drug effect, which are
consistent with the stepping stone hypothesis, but also psychosocial factors that are
independent of drug-specific effects. There is no evidence that marijuana serves as a
stepping stone on the basis of its particular drug effect. One might argue that marijuana
is generally used before other illicit mood-altering drugs, in part, because its effects
are milder, but in that case, marijuana is a stepping stone only in the same sense as
taking a small dose of a particular drug and then increasing that dose over time is a
stepping stone to increased drug use.
- Whereas the stepping stone hypothesis presumes a predominantly physiological component
to drug progression, the gateway theory is a social theory. The latter does not suggest
that the pharmacological qualities of marijuana make it a risk factor for progression to
other drug use. Instead it is the legal status of marijuana that makes it a gateway drug. 81
3.22
- Psychiatric disorders are associated with substance dependence, and are likely risk
factors for progression in drug use. For example, the troubled adolescents studied by
Crowley and coworkers 31 were dependent on an average of 3.2 substances,
suggesting that their conduct disorders are associated with increased risk of progressing
from one drug to another. Substance abuse of a single substance is also a likely risk
factor for subsequent multiple drug use. For example, in a longitudinal study that
examined drug use and dependence, about 26% of problem drinkers report they first used
marijuana after the onset of alcohol-related problems (R. Pandina, IOM workshop). This
study also found that 11% of marijuana users developed chronic marijuana problems,
although most also had alcohol problems.
- Intensity of drug use is also an important risk factor in progression. Daily marijuana
users are more likely than their peers to be extensive users of other substances (for
review see Kandel and Davies 77 ). Seventy-five percent of 34-35 year old men
who had used marijuana 10-99 times by age 24-25 never used any other illicit drug; 53% of
those who had used it more than 100 times did progress to using other illicit drugs 10 or
more times. 77 Comparable proportions for women are 64% and 50%.
- The factors that best predict illicit drug use other than marijuana are likely the
following: age of first alcohol or nicotine use, heavy marijuana use, and psychiatric
disorders. However, it is important to keep in mind that progression to illicit drug use
is not synonymous with heavy or persistent drug use. Indeed, although the age of onset for
licit drug alcohol and nicotine) use predicts later illicit drug use, age of first use of
licit drugs does not appear to predict persistent or heavy use of those drugs. 89
- Data on the gateway phenomenon are frequently over-interpreted. For example, one study
reports that "marijuana's role as a gateway drug appears to have increased"
(Golub and Johnson 1994). This was a retrospective study based on interviews of drug
abusers who reported smoking crack or injecting heroin on a daily basis. Those data
provide no indication of what proportion of marijuana users become serious drug abusers.
Rather, they indicate that serious drug abusers usually use marijuana before they smoke
crack or inject heroin. Only a small percent of the adult population use crack or heroin
on a daily basis; during the five-year period from 1993-1997, an average of three people
per 1000 had used crack and about two per 1000 had used heroin in the past month. 131
- Many of the data on which the gateway theory is based do not measure dependence. Instead
they measure use, even once-only use. Thus those data show only that, compared to people
who never use marijuana, marijuana users are more likely to use those drugs (maybe even
only once), not that they become dependent or even frequent users. Note that the authors
of these studies are careful to point out that their data should not be used as evidence
of an inexorable, causal progression. Rather they note that identifying stage-based user
groups makes it possible to identify the specific risk factors that predict movement from
one stage of drug use to the next - this is the real issue in the gateway discussion. 25
3.23
- In the sense that marijuana use typically precedes rather than follows initiation into
the use of other illicit drugs, it is indeed a gateway drug. However, it does not appear
to be a gateway drug to the extent that it is the most significant predictor or even the
cause of heavy drug abuse; that is, care must be taken not to attribute cause to
association. The most consistent predictors of heavy drug use appear to be the intensity
of marijuana use, and co-occurring psychiatric disorders or a family history of
psychopathology including alcoholism. 77, 82
- An important caution is that data on drug use progression pertain to nonmedical drug
use. It does not follow from those data that if marijuana were available by prescription
for medical use, the pattern of drug use would be the same. Kandel and coworkers also
studied nonmedical use of prescription psychoactive drugs in their study of drug use
progression. 81 In contrast to alcohol, nicotine, and illicit drugs, there was
not a clear and consistent sequence of drug use involving the abuse of prescription
psychoactive drugs. At present, the data on drug use progression neither support nor
refute the suggestion that medical availability would increase drug abuse among medical
marijuana users. It is, admittedly, another question as to whether the medical use of
marijuana might encourage drug abuse among the general community - not among medical
marijuana users themselves, but among others simply because of the fact that marijuana is
used for medical purposes.
The Link Between Medical Use and Drug
Abuse
- Almost everyone who spoke or wrote to the IOM study team about the potential harms of
the medical use of marijuana felt that it would send the wrong message to children and
teenagers. They stated that information about the harms of marijuana is undermined by
claims that marijuana might have medical value. Yet, many of our powerful medicines are
also dangerous medicines. These two facets of medicine -effectiveness and risk - are
inextricably linked.
- The question here is not whether marijuana can be both harmful and helpful, but whether
the perception of its benefits will increase its abuse. For now, any answer to the
question remains conjecture. Because marijuana is not an approved medicine, there is
little information about the consequences of its medical use in modern society. The
following are three examples from which reasonable inferences might be drawn. Opiates such
as morphine and codeine are an example of a class of drugs that is both abused to great
harm and used to great medical benefit, and it 'would be useful to examine the
relationship between medical use and abuse. Another example is the natural experiment
during 1973-1978 in which some states decriminalized marijuana, and others did not.
Finally, one can examine the short term consequences of the publicity surrounding the 1996
medical marijuana campaign in California. Did this have any measurable impact on the
marijuana consumption among youth in California? The consequences of this
"message" that marijuana might have medical use are examined below.
3.24
Medical Use and Abuse of Opiates
- Two highly influential papers published in the 1920s and 1950s led to a widespread
concern among physicians and medical licensing boards that liberal use of opiates would
result in many addicts reviewed by Moulin and coworkers 105 in 1996. Such fears
have proven unfounded; it is now recognized that fear of producing addicts through medical
treatment resulted in needless suffering among patients with pain, as physicians
needlessly limited appropriate doses of medications. 27, 44 Few individuals
begin their drug addiction problems by misuse of drugs that have been prescribed for
medical use. 113 In general, opiates are carefully regulated in the medical
setting and diversion of medically prescribed opiates to the black market is not generally
considered to be a major problem.
There is no evidence to suggest that the use of
opiates or cocaine for medical purposes has increased the perception that the illicit use
of these drugs is safe or acceptable. Clearly, there are risks that patients may abuse
marijuana for its psychoactive effects as well as risks of diversion of marijuana from
legitimate medical channels into the illicit market. Again, this does not differentiate
marijuana from many accepted medications that are abused by some patients or diverted from
medical channels for non-medical use. Where this has taken place, medications have been
placed in Schedule II of the Controlled Substances Act, which brings the drug under
stricter control, including quotas on the amount that can be legally manufactured (see
chapter 5 for discussion of the Controlled Substances Act). This scheduling also signals
to physicians that the drug has abuse potential and that they should monitor the use of
the medication by patients that may be at risk for drug abuse.
Effect of Marijuana Decriminalization
Monitoring the Future, the annual survey of values and life-styles of high school
seniors, revealed that high school seniors in decriminalized states reported using no more
marijuana than did their counterparts in states where marijuana was not decriminalized. 71
Another study reported somewhat conflicting evidence indicating that decriminalization had
increased marijuana use. 104 That study used data from the Drug Awareness
Warning Network (DAWN), which has collected data since 1975 on drug-related emergency (ER)
room cases. Among states that had decriminalized marijuana in 1975-1976, there was a
greater increase from 1975 to 1978 in the proportion of ER patients who had used marijuana
than in states that did not decriminalize marijuana (table 3.6). Despite the greater
increase among decriminalized states, by 1978, the proportion of marijuana users among ER
patients was about equal in states that did and states that did not decriminalize
marijuana. This is because the non-decriminalized states had higher rates of marijuana use
before decriminalization. In contrast to marijuana use, rates of other illicit drug use
among ER patients were substantially higher among states that did not decriminalize
3.25
marijuana use. Thus, there are different possible reasons for the relatively greater
increase in marijuana use in the decriminalized states. On the one hand, decriminalization
might have led to an increased use of marijuana (at least among people who seek health
care in hospital emergency rooms). On the other hand, the lack of decriminalization might
have encouraged greater use of drugs that are even more dangerous than marijuana.
Interpretations are ambiguous.
- The differences between the results for high school seniors from the Monitoring the
Future study and DAWN data are unclear, although the author of the latter study suggests
the reasons might lie in limitations inherent in how the DAWN data are collected. 104
In sum, there is not strong evidence that decriminalization causes a significant increase
in marijuana use.
- In 1976, the Dutch adopted a policy of toleration for possession of up to 30 g of
marijuana. There was little change in marijuana use during the seven years following this
policy change, suggesting that the policy change itself had little impact; however, in
1984 when Dutch "coffee shops" that sold marijuana commercially spread
throughout Amsterdam, marijuana use began to increase. 97 During the 1990s,
marijuana use has continued to increase in the Netherlands at the same rate as in the
United States and Norway two countries that strictly forbid marijuana sale and possession.
Further, during this period, approximately equal percentages of American and Dutch 18-year
olds used marijuana; Norwegian 18-year olds were approximately half as likely to have used
marijuana. The authors of this study conclude that there is little evidence that the Dutch
marijuana depenalization policy led to increased levels of marijuana use, although they
note that commercialization of marijuana might have contributed to its increased use.
- In sum, there is little evidence that decriminalization of marijuana use necessarily
leads to a substantial increase in marijuana use.
3.26
Table 3.6 Decriminalization and Marijuana Use
| Effect of Decriminalization on Marijuana Use in ER Cases |
| . |
Total Reports of Drug Use per ER |
| . |
Time Period (States the decriminalized so after 1975 and before 1978 |
States that decriminalize marijuana. |
States that did not Decriminalized marijuana |
| Marijuana use |
1975 |
0.8 |
1.5 |
| 1978 |
2.7 |
2.5 |
| Other drug use |
1975 |
47 |
55 |
| 1978 |
55 |
70 |
Table legend. The values shown indicate the frequency of drug use among ER patients in
states that decriminalized marijuana from July 1975- July 1977 and in those that did not.
Data are based on patient self-reports. The 1975 values reflect ER marijuana reports
before or in the first months of decriminalization, whereas the 1978 values reflect ER
reports when decriminalization laws had been in effect at least one year. The 1978 levels
are median values for quarters in 1978, and are derived from figures 1 and 2 in Model
(1993). 104 The values in the column for states that did not decriminalize
represent what might have been seen if the states in the first column had not
decriminalized.
3.27
Effect of the Medical Marijuana Debate
- The most recent National Household Survey on Drug Abuse showed that among youth ages
12-17 the perceived risk of smoking marijuana once or twice a week had decreased
significantly between 1996 and 1997. 131 (Perceived risk is measured as the
percent of survey respondents who report that they "perceive great risk of harm"
in using a drug at a specified frequency.) At first glance, this might seem to validate
the fear that the medical marijuana debate of 1996 - prior to the passage of the
California medical marijuana referendum in November 1997 - had sent a message that
marijuana use is safe. But a closer analysis of the data shows that Californian youth were
an exception to the national trend. The perceived risk of marijuana use did not change
among California youth between 1996 and 1997. 131 a. In sum, there
is no evidence that the medical marijuana debate has altered perceptions among adolescents
about the risks of marijuana use. 131 a
Psychological Harms
- In assessing the relative risks and benefits of the medical use of marijuana, the
psychological effects of marijuana may be viewed both as unwanted side effects as well as
potentially desirable end points in medical treatment. However, the vast majority of
research on the psychological effects of marijuana has been done in the context of
assessing the drug's intoxicating effects when used for non-medical purposes. Thus the
literature does not directly address what effects will occur when marijuana is taken for
medical purposes.
- There are some important caveats to consider in attempting to extrapolate from this
research to the medical use of marijuana. The circumstances under which psychoactive drugs
are taken are an important influence on the psychological effects produced. Further,
research protocols to study marijuana's psychological effects in most instances were
required to use participants who had prior experience with marijuana. Clearly, people who
might have had adverse reactions to marijuana would either choose to not participate in
this type of study or would be screened out by the investigator. Therefore, the incidence
of adverse reactions to marijuana that might occur in individuals with no marijuana
experience cannot be estimated from such studies. A further complicating factor concerns
the dose regimen used for laboratory studies. In most instances laboratory research
studies have looked at the effects of single doses of marijuana which might be different
than that observed when the drug is taken repeatedly for a chronic medical condition.
- Nonetheless, laboratory studies are useful in suggesting what psychological functions
might be studied when marijuana is evaluated for medical purposes.
a Although Arizona also passed a medical marijuana referendum, it was
embedded in a broader referendum concerning prison sentencing. Hence the debate in Arizona
did not focus on medical marijuana the way it did m California, and changes in Arizona
youth attitudes likely reflect factors peripheral to medical marijuana.)
3.28
- Laboratory studies indicate that acute and chronic marijuana use has pronounced effects
on mood, psychomotor, and cognitive functions. These psychological domains should,
therefore' be considered in assessing the relative risks and benefits of the therapeutic
use of marijuana or cannabinoids for any medical condition.
Psychiatric
disorders
- A major question remains as to whether marijuana can produce lasting mood disorders or
psychotic disorders such as schizophrenia. Georgotas and Zeidenberg reported that smoking
10-22 marijuana cigarettes per day was associated with a gradual waning of the positive
mood and social facilitating effects of marijuana and an increase in irritability, social
isolation and paranoid thinking. Considering that smoking one cigarette is enough to make
a person feel "high" for about one to three hours, 67, 94, 117 the
subjects in that study were taking very high doses marijuana. Reports have described the
development of apathy, lowered motivation and impaired educational performance in heavy
marijuana users who do not appear to be behaviorally impaired in other ways. 12, 121
There are clinical reports of marijuana induced psychotic-like states (schizophrenia like;
depression and/or mania) lasting for a week or more. 111 Hollister suggests
that because of the varied nature of the psychotic states induced by marijuana, there is
no specific "marijuana psychosis." Rather, the marijuana experience may trigger
latent psychopathology of many types. 65 More recently, Hall and colleagues
concluded that "there is reasonable evidence that heavy cannabis use, and perhaps
acute use in sensitive individuals, can produce an acute psychosis in which confusion,
amnesia, delusions, hallucinations, anxiety, agitation and hypomanic symptoms
predominate." Regardless of which of these interpretations is correct, both reports
agree that there is little evidence that marijuana alone produces a psychosis that
persists after the period of intoxication.
Schizophrenia
- The association between marijuana and schizophrenia is not well understood. The
scientific literature indicates general agreement that heavy marijuana use can precipitate
schizophrenic episodes, but not that marijuana use can cause the underlying psychotic
disorder. 58, 95, 150 As noted earlier, drug abuse is common among people with
psychiatric disorders. Estimates of the prevalence of marijuana use among schizophrenics
vary considerably, but are in general agreement that it is greater than or equal to use
among the general population. 133 Interestingly, schizophrenics prefer the
effects of marijuana over those of alcohol and cocaine, 35 which they generally
use less often than does the general population. 133 The reasons for this are
unknown, but it raises the possibility that schizophrenics might obtain some symptomatic
relief from moderate marijuana use. But overall, compared with the general population,
individuals with schizophrenia or with a family history of
3.29
schizophrenia are likely to be at greater risk of suffering adverse psychiatric effects
from the use of cannabinoids.
Cognition
- As discussed earlier, acutely administered marijuana impairs cognition. 59, 65, 111
PET imaging (positron emission tomography) allows investigators to measure the acute
effects of marijuana smoking on active brain function. Human volunteers who perform
auditory attention tasks before and after smoking a marijuana cigarette show impaired
performance while under the influence of marijuana; this is associated with substantial
reduction in blood flow to the temporal lobe of the brain, an area that is sensitive to
such tasks. 115 116 In other brain regions, such as the frontal lobes and lateral
cerebellum, marijuana smoking increases blood flow. 100, 154 Earlier studies
purporting to show structural changes in the brains of heavy marijuana users 22
(have not been replicated using more sophisticated techniques. 28, 88
- Nevertheless, recent studies 121, 14 have found subtle defects in cognitive
tasks in heavy marijuana users after a brief period (19-24 hours) of marijuana abstinence.
Longer term cognitive deficits in heavy marijuana users have also been reported. 139
Although these studies have attempted to match heavy marijuana users with subjects with
similar cognitive abilities prior to exposure to marijuana use, the adequacy of this
matching has been questioned. 132 A consideration of the complex methodological
issues facing research in this area is well reviewed in an article by Pope and colleagues.
120 Care must be exercised in this area so that studies are designed to
differentiate between changes in brain function caused by the illness for which marijuana
is being given and the effects of marijuana. AIDS dementia is an obvious example of this
possible confusion. It is also important to determine whether the repeated use of
marijuana at therapeutic dosage levels produces any irreversible cognitive effects.
Psychomotor Performance
- Marijuana administration has been reported to affect psychomotor performance on a number
of different tasks. The review by Chait and Pierri 23 details not only the
studies which have been done in this area but also points out the inconsistencies across
studies, the methodological shortcomings of many studies, and the large individual
differences among the studies attributable to subject, situational and methodological
factors. Those factors must be considered when designing studies of psychomotor
performance in participants involved in a clinical trial of the efficacy of marijuana. The
types of psychomotor functions that have been shown to be disrupted by the acute
administration of marijuana include: body sway, hand steadiness, rotary pursuit, driving
and flying simulation, divided attention, sustained attention, and the digit-symbol
substitution test. A study of experienced airplane pilots showed that, even 24 hours after
a single marijuana cigarette, their
3.30
performance on flight simulator tests was impaired (Yesavage and coworkers 1985 162).
Before the tests, however, they told the study investigators that they were sure their
performance would be unaffected.
- Clearly, cognitive impairments associated with acutely administered marijuana limit the
activities that individuals being treated with marijuana would be able to do safely or
productively. For example, no one under the influence of marijuana or THC should drive a
vehicle or operate potentially dangerous equipment.